Epidemiology
Learning objectives
By the end of this session, trainees need to understand the:
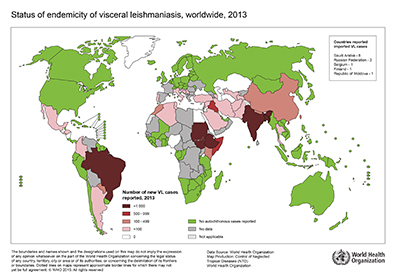
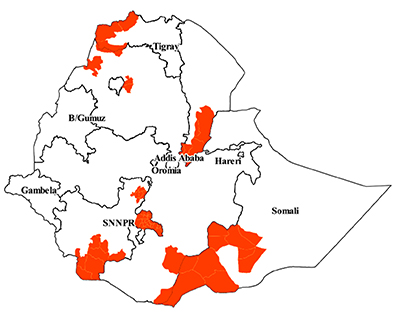
- Global and the national burden of leishmaniasis
- Geographic distribution of the disease
Recommended facilitation technique
- Make participants read the participant manual
- Arrange a team work to study the world and Ethiopia map on the distribution of disease and identify endemic spots, naming the countries and places
Use map on the supplement power point to demonstrate and explain the distribution of the disease
Epidemiology in Ethiopia
References:
Alvar J et al, Leishmaniasis worldwide and Global estimates of its incidence. PlosOne 7 (5) 2012
WHO, weekly epidemiological record. 3 June 2016. No 22, 91 (285-296)
Guidelines for diagnosis, treatment and prevention of leishmaniasis in Ethiopia, 2nd Ed. June 2013
Wondimeneh Y et al. Trend analysis of visceral leishmaniasis at Addis Zemen Health Center, Northwest Ethiopia, Biomedical research international. 2014